Overview
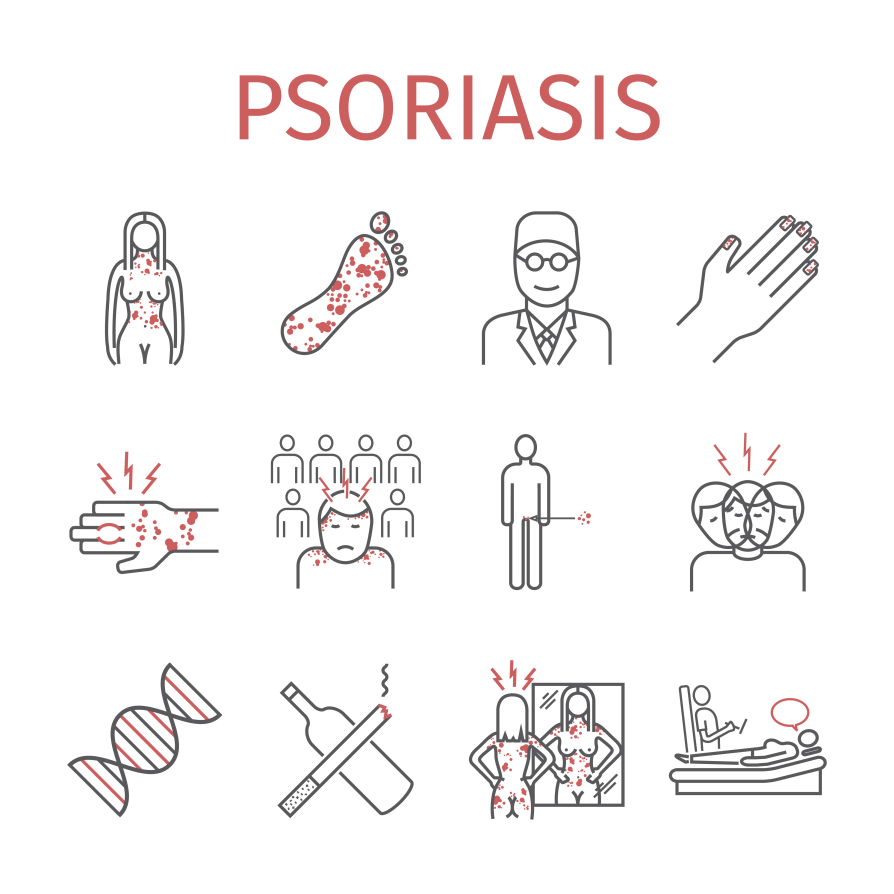
Psoriasis is a skin condition that causes the formation of scales and red patches on the skin.
The word psoriasis is derived from Greek words psora and iasis which can be translated as “itch” and “condition” respectively and can be termed as “itching condition” or “being itchy.”The scales and patches formed due to psoriasis are itchy and painful.
Scales usually are noticed on the joints. However, they spread to other parts of the body, including:
- Feet
- Hands
- Neck
- Face
- Scalp
Less common forms of psoriasis affect the mouth, nails, and the region surrounding the genitals.
Psoriasis is a chronic disease that often shows up and fades away in a repetitive manner. This condition is caused due to rapid cell build up on the surface of the skin. The severity of psoriasis could range from small patches to full body coverage.
According to a study carried out by the World Psoriasis Day Consortium, 125 million people all over the world (2-3 percent of the world’s population) are affected by psoriasis. Other studies state that 10-30 percent of people affected by psoriasis develop psoriatic arthritis, and is also linked with other health conditions, such as:
Types of Psoriasis
- Plaque Psoriasis – This type of psoriasis constitutes to about 90% of the cases. It is characterized by red patches with white scales on the top. This is also called as psoriasis vulgaris. It commonly affects the back of forearms, navel area, scalp and shins. They are also known to occur around the genitals and also on the soft tissue inside the mouth.
- Guttate Psoriasis – This type comes with spots which are small and separate and in the shape of a drop. They affect the body, limbs, face and head.
- Inverse Psoriasis – This type is characterized by the formation of red patches in the folds of the skin. It is also called as flexural psoariasis.
- Pustular Psoriasis – This type of psoriasis forms blisters which are usually filled with pus. The blisters are small and affect hands and feet. The patients may also have accompanying flu-like symptoms.
- Erythrodermic Psoriasis – This can develop from any of the other types of psoriasis. It occurs when the rash becomes widespread, red and scaly. It is a serious form which requires hospitalization.
- Nail Psoriasis – This type involves fingernails and toenails and causes pits and changes in the nail color. Most people experience nail psoriasis at some point in life.
A combination of genetic and environmental factors is known to cause psoriasis. It could occur at any age but is known to commonly appear for the first time between 15 to 25 years of age. The numbers of cases reported are higher in regions that are far from the equator. While the condition is relatively uncommon in African Americans, it is seen to be very common in people with European ancestry. Individuals with irritable bowel syndrom, eulcerative colitis and Crohn’s disease are more vulnerable to psoriasis.
Most patients with psoriasis suffer mild symptoms like mild-skin lesions that can be treated easily and effectively with the use of topical therapies. For cases that range from moderate to severe, the patient may be subject to phototherapy, diet restrictions and other treatment procedures.
Causes of Psoriasis
A number of theories exist on the causes of psoriasis through the precise causes are not fully understood. Factors like the following are believed to play a role in causing psoriasis:
- Genetics – Nearly one-third of patients suffering from psoriasis have acquired the disease genetically. In cases of identical twins where one twin suffers from the condition, the other twin has about 70% chances of displaying symptoms of the disorder sooner in life. The same is reduced to 20% in case of non-identical twins.
- Lifestyle – Factors like stress, the presence of infections, changes in the environment, etc. might worsen psoriasis. Excessive alcohol consumption, obesity, cigarette smoking, dryness of skin, exposure to hot water are known to worsen the condition.
- HIV – Individuals who are HIV-positive are at a higher risk of being affected with psoriasis. The symptoms also tend to be more severe in these individuals. They are also prone to be affected by psoriatic arthritis.
- Microbes -Staphylococcus aureus, Malassezia and Candida albicans can increase the tendency for psoariasis.
- Medications -Drugs like beta blockers, antimalarial medications, non-steroidal anti-inflammatory drugs, calcium channel blockers, lipid-lowering drugs, etc. are known to cause psoriasis. This type of psoriasis is also called as drug-induced psoriasis
Psoriasis is characterized by an abnormal growth of the outer layer of the skin. An overabundance of skin cells and abnormal production of cells during wound repair usually results in psoriasis. The usual time taken for skin-cell replacement is 28 – 30 days. But in the case of psoriasis, skin gets replaced every 3 to 5 days. Premature maturation of keratinocytes is believed to be a reason for this rapid growth.
Psoriasis is an autoimmune condition. In normal conditions, white blood cells are responsible for destroying foreign bacteria and fighting infections. In case of psoriasis, white blood cells are believed to attack skin cells mistakenly. This mistaken attack causes an overdrive in skin cell production, resulting in plaques that are associated with psoriasis.
Apart from other causes, there are a number of factors that trigger psoriasis. Some of the common trigger factors include skin injuries, stress, tension, cold temperatures, a weakened immune system, cuts on the body, bug bite, sunburn, and autoimmune disorders. Triggers can be identified potentially by keeping a track of symptoms and when they occur.
Symptoms of Psoriasis
Symptoms of psoriasis vary from type to type. Each type of psoriasis displays a unique set of symptoms which are in a way characterized by skin lesions, flakes and itchiness.
Common symptoms of psoriasis include:
- Red patches of skin
- Dry, cracked skin
- Hair Removal
- Itchy and burning skin
- Sore lesions
- Pitted nails
- Swollen joints
- Stiff joints
- Dandruff-like eruptions on the skin
Symptoms of different types of psoriasis are as follows:
Plaque Psoriasis Symptoms
- Raised areas of inflamed skin
- Silvery scales
- Itchy and painful lesions
Nail psoriasis Symptoms
- Thickened nails
- Pitted nails
- Abnormal nail growth
- Discoloration of nail
- Loosened nail from the nailbed
- Crumbled nail
Guttate psoriasis Symptoms
- Primarily affects young adults and children
- Water-drop shaped lesions
- Scaling of skin on trunk, arms, legs, scalp
- Sudden eruption of lesions
Inverse psoriasis Symptoms
- Blisters develop quickly
- Pus-filled blisters
- Red and tender skin
- Severe itching
- Fever, chills
Erythrodermic psoriasis Symptoms
- Rash covers the entire body
- Peeling skin
- Intense burning and itching
Psoriatic arthritis Symptoms
- Scaly skin
- Swollen joints
- Painful joints
- Stiffness in joints
Risk Factors Psoriasis
The risk of being affected with psoriasis is higher for some individuals. The risk depends on the following factors.
- Family History: If there has been a case of psoriasis in a family line, the risk of developing the condition is higher.
- Infections: Individuals with autoimmune conditions and infections are more likely to develop psoriasis than those who are healthy.
- Stress: High-stress levels can potentially increase the risk of psoriasis. This is because stress can impact the immune system.
- Habits: Being alcoholic and being under the influence of tobacco could also increase a person’s risk of developing psoriasis. These factors are also known to increase the severity of the disease.
- Obesity: Psoriatic lesions often appear in skin creases and folds. People who are obese are more vulnerable to psoriasis.
Diagnosis
The diagnosis is usually done through two methods. They are:
- Physical Examination: By examining the skin, scalp, and nails of the person, a doctor can usually diagnose psoriasis. While noting all this, his/her medical history would also be taken into consideration to see if there has been a case of psoriasis in the family line.
- Skin biopsy: Under rare circumstances, a biopsy could be ordered for the skin. A small sample of the skin would be taken to perform the biopsy. The sample is then examined under a microscope to understand the type of psoriasis that has occurred. This is also used to rule out other possible disorders.
Treatment
Treatment of psoriasis can be divided into four main types. They are topical treatments, light therapy medication and alternative medicine.
Topical Treatments
For patients with mild to moderate disease, topical application of creams and ointments can effectively treat the condition. For severe cases, this is used in combination with oral medicines or light therapy.
Topical treatment of psoriasis includes use of topical corticosteroids, vitamin D analogs, anthralin, topical retinoids, calcineurin inhibitors, salicylic acid, coal tar and moisturizers.
Light Therapy
This treatment uses natural or artificial UV light to treat psoriasis. Exposing the skin to controlled amounts of natural sunlight also comes under light therapy. UV A and UV B lights are also used to treat psoriasis. Light therapies like narrow-band UVB phototherapy, Goeckerman therapy, psoralen plus UVA therapy, excimer laser therapy, etc. are well-known therapies that use light and its forms to treat psoriasis.
Medications
Use of oral and injected medication is necessary if a person has severe psoriasis or if he is resistant to other treatment types. This type of treatment is also called systemic treatment. Drugs like retinoids, methotrexate, cyclosporine, and other drugs that alter the immune system are used in treating psoriasis.
Alternative Medicine
Apart from generic medicines that treat psoriasis, there are several alternative therapies that are proven to reduce symptoms of psoriasis. Such alterations include special diets, use of dietary supplements, herbs and creams. These treatments are not as effective as other treatment procedures but are considered safe for long-term usage. They are believed to ease symptoms like itching, scaling and pain. This treatment could be the best choice for patients with mild psoriasis.
Remedies like usage of aloe-vera, fish oil and Oregon grape are also well-known in treating psoriasis. Application of aloe-vera cream has shown to reduce scaling, itching and inflammation. This can be used on a repetitive basis and as required by the patient to see significant improvement. Omega -3 fatty acids that are found in fish oil also reduce inflammation associated with psoriasis. Topical application of Oregon grape which is also known as barberry has also shown to reduce inflammation and ease a psoriatic condition.
Prevention
The measures that could aid in the prevention of psoriasis include –
- Daily Bath: Taking a bath every day helps remove inflamed skin and scales. Adding oils and salts to the bath could be more beneficial. Usage of hot water, harsh soaps can trigger the symptoms.
- Moisturize: It is important to moisturize the skin after every bath. Using thick creams would help keep the skin moist and soft. Preventing the skin from getting dry would keep it from forming scales.
- Light Exposure: Exposing oneself to a controlled amount of sunlight could keep the skin healthy. The exposure, if too much, can cause adverse effects.
- Avoid Triggers: Taking steps to avoid triggering factors that cause psoriasis also helps in the prevention of psoriasis. Keeping the skin protected from injuries and infections would also be beneficial.
- Avoid Alcohol: Usage of alcohol would interfere with the treatment of psoriasis. For individuals who already suffer from psoriatic conditions, it is important to refrain from alcohol.
FAQs
Is psoriasis contagious?
No. Psoriasis cannot be passed by touching a skin lesion.
How can someone get psoriasis?
A person can develop psoriasis when his immune system sends wrong signals that lead to increases in skin cell production. The excessive cells pile up on the surface of the skin, leading to scaly patches that are itchy and painful.
Can foods trigger psoriasis?
Yes. Certain foods like processed meat, dairy product, red meat, etc. also trigger psoriasis.
What kind of creams can be used to treat psoriasis?
Thick lotions and creams that seal the moisture are good for psoriasis treatment. Application of petroleum jelly, olive oil and other thick substances which keep the skin moist often help in treatment.