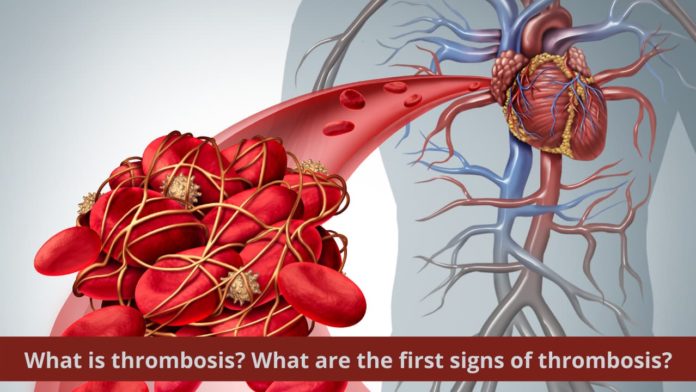
Most of us hurt ourselves in some or the other way and bleed. After a certain period, the blood from the site of the cut stops, and we see a rough mass of blood. That hard mass is known as a blood clot or thrombus. The formation of a blood clot is crucial for the body. This mechanism is necessary for our body, or else we would be blood deficient right now. So when does it become harmful for us? When the blood clot forms inside a blood vessel, it disturbs the normal functioning of your circulatory system. The blood cannot flow expectedly and is known as thrombosis. Thrombosis comes from the word thrombus that means blood clots.
What is thrombosis?
Venous thromboembolism is when a blood clot forms inside your veins. It results in deep vein thrombosis (DVT) and may result in pulmonary embolism. Alternatively, atherothrombosis is when blood clots form within the arteries that leads to stroke and heart attack. Deep vein thrombosis can cause severe leg pains, swelling, and happens due to some medical conditions, surgery, or prolonged bed rest. These blood clots may travel throughout your bloodstream and deposit in your lungs, blocking the flow of blood. It is known as pulmonary embolism. Ultrasound can diagnose this condition.
Be aware of the first signs of thrombosis so you can seek urgent medical care.
What are the signs and symptoms of thrombosis?
The signs of thrombosis can be painful or uncomfortable . They are:
- Heaviness in legs , unbearable pain with cramps and soreness
- Discomfort and itching throughout your leg
- Frequent aches and a warm feeling in the leg
- Discoloration, thickening, or ulceration of skin in the leg
- Swelling in the leg
Deep vein thrombosis carries the risk of pulmonary embolism.
Symptoms of pulmonary embolism are no less discomforting. They can include:
- Shortness of breath
- Chest pain and pain while deep breathing
- Pain in the chest while coughing
- Fatigue and weakness, dizziness, fainting
- Pulse rate increases rapidly
- Cough with traces of blood
When to see a doctor?
Contact your doctor if –
- You witness the first few signs of deep vein thrombosis, like leg pain, swelling, and discoloration.
- You are experiencing discomfort in the chest and a feeling of heaviness.
- You see symptoms of pulmonary embolism. Pulmonary embolism is a life-threatening complication of DVT.
Call 1860-500-1066 to book an appointment
What can cause thrombosis?
Thrombosis, the formation of a blood clot within a blood vessel, can result due to any of the following reasons:
- Injury to a vein or artery,
- Soon after surgery,
- Severe accident,
- Limited movement of the leg due to bed-rest, and
- Some medications
Also Read About: Blood Clot in the Brain
What increases the risk of thrombosis?
Several factors increase the risk of developing deep vein thrombosis. They are as follows:
- Immobilization of leg
This process occurs if the joint or bone is in a cast or brace to prevent any injury. The prolonged bed rests limits the ability of calf muscles to contract that results in DVT.
- Hypercoagulability
It is also known as thrombophilia. It results in increased blood clot formation. The standard process is known as coagulation, and the increased tendency is known as hyper-coagulation.
- Surgical operations
Surgeries of knees and other orthopedic surgery increase the risk of thrombosis.
- Pregnancy
When you are pregnant, the entire weight or pressure goes into your veins of the pelvic region and legs. This risk does not end after giving birth; it persists for six weeks even after the delivery.
Being overweight has the same effect as pregnancy has on your legs. Increased pressure in your legs and pelvic region can cause DVT.
- Oral contraceptives
Birth control pills or hormone replacement therapy (HRT) can increase blood coagulation.
- Smoking
- Cancer
Few types of cancer and cancer treatment increase blood coagulation.
IBD can increase the risk of DVT.
- Age
DVT can occur at any age, but people aged 60 or above are at a higher risk.
What are the treatment options for deep vein thrombosis?
- Anticoagulants
Using anticoagulants is the most common treatment for deep vein thrombosis. They are also known as blood thinners. These pills and injections decrease blood’s ability to clot. Some of the blood thinners are:
- Your doctor will give heparin intravenously, that is, through injection in your arm’s vein. They can also use enoxaparin, fondaparinux, and dalteparin similarly.
- The doctor may give warfarin and dabigatran after injections. Pregnant women should avoid taking blood thinners.
- The doctor may prescribe other blood thinners. They are rivaroxaban, edoxaban, and apixaban. In this case, you will not need intravenous medicines.
Your doctor might recommend clot busters, filters, and compression stockings depending upon the severity, inability to take medicines, or to help prevent swelling. Compression stockings can be worn for at least two years in the daytime to help reduce the clotting.
Call 1860-500-1066 to book an appointment
What are the complications of thrombosis?
- Pulmonary embolism
A life-threatening complication of deep vein thrombosis is pulmonary embolism (PE). It occurs when the blood clot in the vessel reaches your lungs from legs and blocks them. It is necessary to watch out for signs and symptoms of pulmonary embolism to prevent it at earlier stages.
- Postphlebitic syndrome
It is the most common complication of DVT. It is also known as post-thrombotic syndrome.
How can you prevent thrombosis?
There are some measures one need to follow to prevent deep vein thrombosis from occurring:
- Limiting prolonged sitting can reduce your chances of thrombosis. Try to keep leg movements going soon as possible after surgery or bed rest. Avoid crossing legs while sitting and stop to walk every hour if on a long drive. If traveling by a plane, raise your heels while resting your toes on the floor to exercise your legs.
- A healthy lifestyle will not only prevent thrombosis but other diseases too. We advise you to lose weight (if overweight) and quit smoking.
- Do regular exercise to reduce the risk of blood clots in vessels.
Conclusion
Deep vein thrombosis requires medical treatment as soon as it is diagnosed. Once your doctor finishes the treatment of DVT, it is your responsibility to make some healthy changes in your lifestyle. Watch out for signs and symptoms . Do not miss follow up with your doctor. Your doctor will assess your condition in the follow-up consultation to modify your treatment if needed. Frequent blood tests will see how well your blood clots after the treatment.
Frequently asked questions
- What are the side-effects of anticoagulants?
Anticoagulant medications are the best treatment option for deep vein thrombosis. Even so, it comes with some risks. There is an increased risk of bleeding after taking anticoagulants. Seek immediate medical attention if you witness nose bleeding, vomiting, bleeding gums, or heavy menses soon after taking prescribed medicines.
- Can my blood clot become recurrent?
The chances of this to be happening are very low if your first clot was due to a surgical procedure or trauma. Although, if you stop your treatment within six months for an unprovoked blood clot, chances of recurrence are near 20 to 30 percent.
Call 1860-500-1066 to book an appointment