Asthma is a chronic respiratory condition characterized by swelling and narrowing of the airways, which may produce excess mucus. Due to this, people experience difficulty breathing, notice wheezing sounds when breathing in, and experience shortness of breath. It can also trigger coughing.
Types of Asthma
Asthma can be of different types based on its severity and triggering factors.
Based on severity, it can be grouped into:
- Mild intermittent
- Mild persistent
- Moderate persistent
- Severe persistent
Based on the triggering factor, this chronic condition can be of the following types:
- Bronchial: This is the most common type and affects the bronchi in the lungs.
- Allergic: It is caused due to allergens such as pet dander, food, mold, pollen, etc.
- Intrinsic: This type is caused due to irritants in the air we breathe, such as cigarette smoke, viral diseases, cleaning products, perfumes, air pollution, etc.
- Occupational: It is caused due to triggering factors in the workplace such as gases, chemicals, dust, or latex.
- Nocturnal: As the name suggests, in this type of asthma, the symptoms worsen at night.
- Cough-variant: This type is characterized by symptoms such as a persistent, dry cough.
- Seasonal: This type occurs only at certain times of the year or in certain conditions such as cold air in winter, pollen during hay fever, etc.
Causes of Asthma
Asthma has a genetic as well as an environmental component. A complex interplay between these two factors causes this chronic disease. Some common causes include:
- If one or both parents of an individual have asthma, they become susceptible to it.
- A prolonged childhood history of viral infections may cause this condition.
- Frequent contact with allergens and irritants could trigger asthma. Common indoor allergens include dust mites, animal proteins, dander from pets, toxic fumes from household cleaners, fungi spores, paint, and cockroaches.
- Excessive exposure to cold and dry air may trigger this condition.
- Strong emotions such as shouting, laughing, crying, etc., and stress can trigger asthma.
- It may be triggered due to workplace irritants such as gases, dust, or chemical fumes.
- Smoggy environmental conditions, high humidity, and intense air pollution tend to cause higher occurrence and recurrence.
- Smoking cigarettes and other forms of tobacco lead to an increased risk of developing the condition.
- Respiratory diseases such as flu and pneumonia trigger a flare-up.
- In some cases, participating in physical activities and exercises could trigger an attack.
- In their childhood, boys are more likely to develop asthma than girls. However, in adulthood, women develop the condition more frequently than men.
- Adults and children who are obese or overweight are more likely to develop this condition.
- Certain medications like aspirin, beta-blockers, naproxen (Aleve), and ibuprofen (Motrin IB, Advil, others) may cause this condition.
- Preservatives and sulfites are added to various types of beverages and foods such as dried fruit, shrimp, beer, processed potatoes, and wine.
- Gastroesophageal reflux disease (GERD) is a condition in which acids from the stomach go back into the throat.
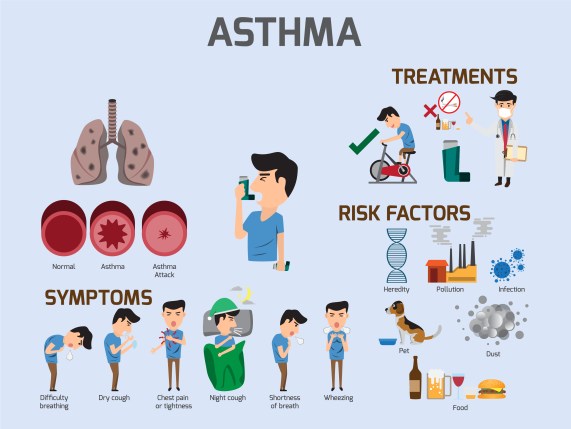
What are its Risk Factors?
Despite the many cited causes of this condition, it is still unclear to researchers why some people develop the condition while others do not. However, some risk factors that can increase your risk of developing asthma include:
- Family history of the condition or allergy—individuals with a blood relative with this condition, such as a parent or sibling.
- Allergic conditions like allergic rhinitis (hay fever) or atopic dermatitis.
- Being overweight or obese.
- Smoking and exposure to second-hand smoke.
- Exposure to exhaust fumes or other types of pollution.
- Exposure to occupational triggers like chemicals used in hairdressing, farming, and manufacturing.
- Exposure to allergens.
- Exposure to chemical irritants.
- Exposure to drugs like aspirin, NSAIDs.
- Low birth weight babies have a high chance of developing the condition.
- Respiratory infections.
- Weather.
- Extreme physical exercise.
A rise in the urban population has been linked to an increase in the incidence and prevalence of asthma.
Symptoms
There are four primary symptoms of asthma. These include:
- Cough
- Wheezing with exhalation (a high-pitched whistling sound due to turbulent airflow through narrow airways).
- Shortness of breath.
- A tight feeling in the chest.
Other symptoms of asthma include
- A cough that worsens at night.
- The symptoms are usually episodic, and individuals can go for long periods of time without any symptoms.
- Common triggers for asthmatic symptoms include exposure to allergens (dust mites, pets, molds, cockroaches, and pollen), viral infections, and exercise.
- Many of the signs and symptoms are usually nonspecific and are also seen in other conditions.
- Symptoms that might suggest conditions other than asthma are the presence of associated symptoms (such as palpitations, chest discomfort, fatigue, and lightheadedness), new symptom onset in older age, and lack of response to appropriate medications for asthma.
- Increased heart rate, increased respiratory rate, and the effort required for respiration.
- Use of accessory muscles to breathe with diminished breath sounds.
- Below normal oxygen level in human body. A low blood oxygen level is a dangerous sign signifying respiratory failure.
- Agitation
- Decreased lung function.
- Difficulty sleeping due to the symptoms mentioned above.
In some individuals, the symptoms of asthma may get aggravated, or flare-ups may occur in the following cases:
- High-intensity or excessive exercising.
- Exposure to irritant gases, chemical fumes, or dust due to occupational conditions.
- Exposure to allergens like pollen, pet dander, spores, etc.
When to See a Doctor?
In most people, asthma is not serious or severe. Though the condition has no cure, it is easily manageable with specific lifestyle changes and management tips, allowing people to live a good quality and healthy life. While most people experience minor flare-ups occasionally, some cases require a visit to the doctor, usually on an emergency basis. Any delay in seeking emergency treatment for the following symptoms of asthma can be potentially life-threatening:
- If you are facing shortness of breath that is rapidly worsening.
- If you do not feel relieved even after using an inhaler.
- If you are experiencing severe shortness of breath while performing day-to-day activities.
.
Call 1860-500-1066 to book an appointment.
Other situations that necessitate visiting your doctor include:
- If you are an asthmatic patient.
- To get your asthmatic condition monitored after diagnosis.
- If you see your asthma getting more severe.
- To get your treatment reviewed.
Complications of Asthma
Asthma is a chronic disorder, and it will coexist with you. If you do not take the right precautions and preventive measures, some complications that you may experience are:
- Trouble sleeping due to wheezing and coughing.
- Missing school, college, or work due to flare-ups.
- Side-effects due to the long-term use of inhalers and medications.
How is Asthma Diagnosed?
An asthma diagnosis is largely based on medical history and a thorough physical examination. People who have this condition also usually have a chronic history of allergic rhinitis, allergies, wheezing, coughing, and difficulty breathing during exercise or when lying down at night. When these conditions are relieved by medication, it is indicative that the person suffers from asthma.
Some diagnostic procedures aid in the diagnosis include:
- Spirometry: It is used to measure the functioning of a lung as the person breathes into a tube. If the person’s lung functioning improves after the administration of a bronchodilator such as albuterol, this confirms the diagnosis of asthma.
However, it is important to note that normal lung function testing does not rule out the possibility of the condition.
- Measurement of exhaled nitric oxide (FeNO): It is performed by a simple breathing exercise. Increased levels of exhaled nitric oxide suggest “allergic” inflammation, which is seen in asthma.
- Skin testing for common aeroallergens: The presence of sensitivities to environmental allergies increases the likelihood of asthma. Skin testing is useful to detect allergies to environmental substances.
- Methacholine challenge test: This test detects hyper-responsiveness of the airway. The tendency of the breathing tubes to narrow in response to irritants is called hyper-responsiveness.
- Sputum eosinophils: This is another marker for “allergic” inflammation seen in chronic conditions like asthma.
- Chest imaging: This imaging test that may show hyperinflation and help rule out other conditions, such as cardiac testing, is also used in certain cases.
- Blood testing: This helps differentiate the types of asthma. Blood tests help to know the level of allergic antibody (IgE) or specialized white blood cells called eosinophils associated with allergic or extrinsic asthma.
Treatment for Asthma
Since asthma cannot be cured, the goals for asthma treatment include:
- Adequate symptom management.
- Reduce trigger factors.
- Maintain normal lung function.
- Maintain normal activity and quality of life.
- Medications prescribed should have minimal side effects.
The treatment for this condition usually involves long-term medications, first-aid or quick-relief, breathing exercises, and home remedies. Depending on your condition, overall health, age, and trigger factors, your doctor will determine the best treatment plan for your asthma.
Various classes of drugs are used as medications, and these can be grouped into long-term medications and quick-relief medications.
The most effective anti-inflammatory agents are the inhalation corticosteroids (ICS) and are considered first-line. ICS is recognized as very effective in decreasing the risk of asthma exacerbations. The combination of an ICS and long-acting bronchodilator (LABA) has a significant beneficial effect on improving asthma control.
Commonly used medications used for this condition are:
- Short-acting bronchodilators (Albuterol) help give quick relief and can be used in conjunction with exercise-induced symptoms.
- Inhaled steroids (budesonide, fluticasone, mometasone, beclomethasone, flunisolide, ciclesonide) are first-line anti-inflammatory therapy.
- Long-acting bronchodilators (formoterol, salmeterol, vilanterol) are added to ICS as additive therapy.
- Leukotriene modifiers zafirlukast, (montelukast, zileuton) serve as anti-inflammatory agents.
- Anticholinergic agents (ipratropium bromide, tiotropium) can help decrease sputum production.
- Anti-IgE treatment (omalizumab) can be used in the allergic type.
- Anti-IL5 treatment (mepolizumab, reslizumab) can be used in eosinophilic asthma.
- Chromones (cromolyn, nedocromil) stabilize mast cells (allergic cells) but are rarely used in clinical practice.
- Theophylline helps in bronchodilation (open the airways) but is rarely used in clinical practice due to an unfavorable side-effect profile.
- Systemic steroids (prednisone, prednisolone, methylprednisolone [Solu-Medrol, Medrol, dexamethasone) are anti-inflammatory medicines used to treat flare-ups but have many side effects.
- Monoclonal antibodies will be available within the next couple of years to treat this condition.
- Immunotherapy or allergy shots decrease the use of medication in allergic forms of the condition.
- Medications are usually administered via inhaler or nebulizer solution. Smoking cessation or minimizing exposure to smoke is essential in treating asthma. Treating conditions such as allergic rhinitis and gastroesophageal reflux disease (GERD) improves symptom control. Vaccinations for influenza and pneumonia are given to prevent exacerbations.
- Though many patients with asthma are treated as outpatients, severe exacerbations are managed in the emergency department. These patients require supplemental oxygen, administration of systemic steroids, bronchodilators such as a nebulized solution. Patients with poor outcomes are referred to a specialist (pulmonologist or allergist).
While some of these are for short-term use, others are long-term medications that need to be taken daily to prevent the symptoms of asthma. These include inhaled corticosteroids, leukotriene modifiers, beta-agonists, combination inhalers, and theophylline.
Quick-relief/first-aid medications are drugs used to provide rapid, short-term relief from symptoms of asthma. These may also be recommended by the doctor to be taken before exercises or strenuous activities. These include nebulizers and rescue inhalers that help you inhale medicines deep into your lungs during flare-ups. Bronchodilators help relax the tightened muscles of your lungs. Anti-inflammatories help target and fight the inflammation in your lungs.
Breathing exercises are very useful in managing asthma in the long term. These exercises help you pass more air in and out of your lungs. Over time, breathing exercises help increase lung capacity and fight severe symptoms of asthma.
Home remedies: Some home remedies are effective in relieving symptoms from escalating and may come in handy. Coffee and caffeinated teas help to open up airways and ease symptoms for up to four hours. Inhaling essential oils, such as eucalyptus, lavender, basil, also helps relieve your symptoms.
Home Remedies for Asthma
Many home remedies can help manage your asthma. Some effective remedies include:
- Ginger: Cut ginger into small pieces and add it to boiling water. Allow it to stay for five minutes. Drink it after it cools.
- Mustard oil: Heat some mustard oil with little camphor. After it cools, rub it on the chest.
- Figs: Soak 3 figs in water overnight. In the morning, eat the figs and drink the water.
- Garlic: Boil 3 cloves of garlic in a glass of milk, and drink it after it cools.
- Coffee: Coffee is a great bronchodilator.
How Can You Prevent Asthma?
Asthma cannot be prevented. However, there are many ways of managing and preventing it from aggravating into a serious, life-threatening episode. Your physician or pulmonologist will devise a management plan for you that will include the following preventive measures:
- Follow the asthma action plan: With the help of your doctor and the healthcare team, take your prescribed medications to manage an asthma attack. It is an ongoing illness that requires regular monitoring and treatment.
- Get vaccinated for influenza and pneumonia: Vaccinations for flu and pneumonia are given to prevent flare-ups.
- Identify and avoid triggers: Several allergens and irritants ranging from pollen to air pollution will trigger attacks.
- Monitor your breathing: The home peak flow meter is used to measure and record the peak airflow. Coughing, wheezing, or shortness of breath are recognized as warning signs of an attack, and immediate action should be taken.
- Identify and treat attacks early: A person is less likely to have a severe attack if attacks are detected and treated early. When your peak flow measurements decrease, it is an alert of an oncoming attack. Take your medications as instructed and immediately stop any activity that may have triggered the attack. If your symptoms don’t improve, get medical help as directed in your action plan.
- Take the medication as prescribed: Just because your symptoms seem to be improving, never change a medication without a doctor’s opinion. It’s a good idea to carry the medications for every medical visit so that the doctor will double-check the use of medications and help you take the right medication.
- Pay attention to increased use of the quick-relief inhaler: If a person notices an increase in the use of a quick-relief inhaler, such as albuterol, it indicates that asthma is not under control. Your doctor will adjust the treatment.
Precautions to Take During the COVID-19 Pandemic
People with comorbidities are said to be in the high-risk category for COVID-19. With both illnesses being respiratory conditions, COVID-19 can cause significant and severe illness in people suffering from asthma. So people with this chronic respiratory condition need to take the following precautions to protect themselves from COVID-19:
- Stay home as much as possible to reduce your risk of exposure.
- Stock up on your medical supplies.
- Maintain social distance with others every day.
- Keep away from others who are sick.
- Clean your hands often with soap and water or use alcohol-based hand sanitizers.
- If someone in your home is sick, separate them from the rest of the family to reduce the risk of a COVID-19 infection.
- Clean and disinfect things touched frequently by you or your family. If possible, have someone who does not have asthma do the cleaning and disinfecting work at home.
- Clean and disinfect surfaces such as phones, remotes, tables, doorknobs, light switches, countertops, handles, desks, keyboards, toilets, faucets, and sinks daily.
- Do not share personal household items such as cups and towels.
Along with taking these precautions, you must also stick to your asthma plan charted out by your doctor and healthcare team, which include:
- Continue your current medicines, including any inhalers with steroids (or corticosteroids) in them.
- Do not stop any medicines or change your treatment plan without talking to your treating doctor.
- Discuss any concerns about your treatment with your doctor.
- Know how to use your inhaler.
- Avoid any potential triggers.
- Strong emotions caused by COVID-19 can trigger an attack. Take steps to cope with your stress and anxiety. Call your treating doctor to know how to deal with your fears.
Conclusion
Asthma is an extremely common chronic condition. It is an illness where the airways swell, and bronchial tubes narrow due to extra mucus production, and the muscles contract making normal breathing difficult. To some, it can be a minor difficulty, whereas to others, it can result in a life-threatening asthmatic attack.
This chronic condition requires a medical diagnosis and is entirely treatable by medical professionals. It usually causes difficulty breathing, pain in the chest, coughing, and wheezing. Flaring up of symptoms is common among asthmatic patients. With proper asthma action plans and timely medications, asthma can be controlled effectively.
Frequently Answered Questions
How can I avoid asthma triggers?
Here are some ways by which you can stay clear of triggers:
- Using an air conditioner to lessen the number of airborne allergens.
- Decontaminating the décor and keeping your home and surroundings clean and hygienic.
- Maintaining optimum humidity with the help of a dehumidifier.
- Preventing the growth of mold spores by cleaning your bathrooms regularly.
How to measure peak flow rate?
You can easily measure your peak expiratory flow rate (PEFR) by handheld devices such as a peak flow meter. This device will measure the ability of your lungs to push the air out of them. Your healthcare provider will advise you regarding the type of peak flow meter to use.
What are some major side effects of bronchodilators?
Nervousness, rapid heartbeat, tremors, and frequent headaches are some major side effects of bronchodilators and quick-relief asthma medications. These side effects worsen with oral forms than with inhaled ones.